I am a Patient
General Purpose Radiography
- Get X-ray examination done only in X-ray facilities Licenced with AERB.
- Do not crowd the room where X-ray is taken. Wait for your turn.
- Co-operate with the radiographer, to avoid repeat X-ray examination.
- If you need to be assisted by your relative during X-ray examination, ask for lead apron for your relative. In no case pregnant woman should assist the patient during exposure.
- Female patient, if pregnant, must inform the radiographer so that necessary precaution can be taken during X-ray examination.
- Carry your old X-ray/CT records.
- Get X-ray examination done only in X-ray facilities Licenced with AERB
- Do not crowd the room where CT is taken. Wait for your turn.
- Co-operate with the Technologist, to avoid repeat CT-scans.
- If you need to be assisted by your relative during X-ray examination, ask for lead apron for your relative. In no case pregnant woman should assist the patient during exposure.
- Female patient, if pregnant, must inform the CT Technologist so that necessary precaution can be taken during CT examination.
- Carry your old X-ray/ CT records.
- Get X-ray examination done only in X-ray facilities Licenced with AERB.
- Co-operate with the operator, to avoid repeat dental X-ray examination.
- Female patient, if pregnant, must inform the operator so that necessary precaution can be taken during dental X-ray examination. .
- Carry your old dental X-ray records.
- Get Interventional Radiology/ Fluoroscopy procedures done in facility Licenced with AERB.
- Ask for radiation exposure record from the hospital/facility.
- Keep a record of the exposures you have received, for future reference. .
- Inform the Technologist if you are pregnant. .
-
Get X-ray examination done only in X-ray facilities Licenced with AERB.
-
Carry your old X-ray records.
What is Radiotherapy?
Radiotherapy is modality of medical treatment using ionising radiation such as gamma rays (emitted from radioactive source), high energy X-rays (generated by medical accelerator) and particle therapy using Hadron Therapy Accelerator (e.g. Proton/ Carbon Ion based).
Why Radiotherapy is usually delivered in fractions?
In radiotherapy, aim is to deliver intended radiation dose to the tumour and minimum possible dose to the surrounding normal tissue. While delivering the dose to the lesion, normal cells surrounding the lesion also receive the unavoidable radiation dose. So radiation doses in Radiotherapy are delivered in fractions which allow to recover these normal cells in between the fractions.
However, it is the prerogative of the Radiation Oncologist to decide the fractionation scheme.
What are the types of Radiotherapy?
In radiotherapy, the radiation dose is delivered to the tumour either by external beam therapy (i.e. teletherapy) or brachytherapy or in combination of both depending on necessity of the case. In the external beam radiation therapy, the radiation dose is delivered to the tumour from a teletherapy unit where radiation source is kept at a certain distance from the tumour. Brachytherapy is a method of cancer treatment in which radiation sources are kept at a short distance from the tumour to deliver radiation dose by interstitial, intracavitary or surface application.
What are the types of Radiotherapy equipment used?
Teletherapy: Equipment used in teletherapy are Telecobalt, Medical Accelerator, Tomotherapy, Cyber Knife and Gamma Knife, Hadron Therapy Accelerator etc. Treatment by proton beam is also an example of Teletherapy.
Brachytherapy: High Dose Rate (HDR)/ Low Dose Rate (LDR) Brachytherapy machines using Co-60/Ir-192 radioactive source and Intra-Operative Radiotherapy (IORT). In Manual Brachytherapy sources used are I-125, Ru-106, Au-198, Pd-103, Sr-90, Ir-192, Co-60 etc
What are treatment techniques available in Radiotherapy?
Treatment techniques available in Radiotherapy are Conventional Radiotherapy, 3D-CRT, IMRT (Intensity-modulated radiation therapy), IGRT (Image-guided radiation therapy), VMAT (Volumetric Arc Therapy), SRS (Stereotactic Radiosurgery) / SRT (stereotactic radiation therapy)/ SBRT (Stereotactic Body Radiation Therapy) etc.
Why Treatment Simulation required in Radiotherapy?
Treatment Simulation is a process in which treatment conditions such as positioning of the patient, patient immobilization, field size, field orientations etc are simulated prior to actual radiation dose delivery in Radiotherapy. The simulation is performed either using conventional simulator or Computed Tomography (CT) Simulator equipment which uses low energy X-rays (kV range).
How can I get list of Radiotherapy Centres?
The list of AERB Licenced Radiotherapy centres across India can be viewed/check in AERB website.
Who are involved in Radiotherapy and what are their responsibilities?
Radiotherapy is a team work which primarily comprises of (i) Radiation Oncologist, (ii) Medical Physicist and (iii) Radiotherapy Technologist.
- Radiation oncologist: Radiation Oncologist is responsible for the overall care of the patient. The responsibilities shall include:
- consultations with the patient, clinical evaluation of the disease and selection of appropriate treatment equipment/ technique for the proposed line of treatment;
- establishment of treatment plan, including dose prescription;
- executions of treatment and participation in it on a regular basis;
- on-treatment evaluations and patient monitoring;
- preparation of treatment summary at the end of the treatment procedure; and
- evaluation of the treatment and follow-up.
- Medical Physicist: Medical Physicist is responsible for:
- facility design and planning calculations, in accordance with the requirements of the installation that meets the regulatory stipulations of radiation protection and safety;
- preparations of specifications for treatment and dosimetric equipment;
- acceptance testing, commissioning and quality assurance (including calibration of therapy equipment);
- periodic calibration of the dosimetric equipment, traceable to national standards laboratory;
- measurement and analysis of beam data; and tabulation of beam data for clinical use;
- evaluation and optimisation of treatment planning;
- development of QA protocols and procedures in radiation therapy regarding
- delivery of radiation treatment, radiation safety and control and regulatory compliance; and
- supervision of radiation therapy equipment servicing and maintenance of records.
- Radiotherapy Technologist: Radiotherapy Technologist is responsible for the following:
- patient set-up strictly in accordance with the prescription chart;
- selection of treatment parameters on the machine and the treatment control panel as defined in the prescription chart;
- delivery of correct dose to the planning treatment volume;
- stopping the treatment, when a fault condition develops;
- intimating the licensee/RSO immediately regarding the incident;
- ensuring that no further treatment is given to the patient, unless the RSO certifies, in writing, that the fault condition has been rectified, and it is safe to commence the treatment after re-setting of the treatment parameters on the control panel; and
- following the radiation safety instructions, specified by the RSO from time to time.
The name ‘nuclear medicine’ may sound frightening to some, but it simply comes from the fact that it is a branch of medicine that employs nuclear radiation – natural emissions from the nucleus of radioactive atoms for either diagnostic or therapeutic procedures It may sometimes go under other names such as ‘radioisotope scanning’ or ‘gamma camera unit’.
Nuclear medicine uses radioactive substances (radiopharmaceuticals) to identify any disorder. A radiopharmaceutical is a chemical (which determines where it goes to in the body) attached to a radioactive label (which allows it to be detected externally). Radiopharmaceuticals can be administered to patients in several ways, including intravenous injection, inhalation and ingestion. Pathology is demonstrated by the site and amount of radiopharmaceutical which accumulates in specific areas within the body. The radioactive label is carefully chosen so that it decays away quite rapidly (usually with a half-life of a few hours). The radioactive label emits radiation which can be detected by a scanner to make an image of where the radiopharmaceutical has accumulated in the patient. Examples of nuclear medicine scanner technologies include the gamma camera and the Positron Emission Tomography (PET) scanner. The nuclear medicine images can be used to assess the amount of radiopharmaceutical taken up into a specific pathological site, which can be valuable for assessing the severity of any pathology. Nuclear medicine uses a wide range of different radiopharmaceuticals and each has specific targeting properties for different organs or physiological pathways.
The radiation dose that a patient receives from a diagnostic nuclear medicine procedure is very small and is about the same as the unavoidable amount of radiation that everyone receives from natural background radiation each year. Nevertheless, for the protection of patients, a firm clinical justification that the benefit will outweigh the risk must be given before a procedure using ionising radiation is conducted. This justification will be done by nuclear medicine staff who understand the risks involved, but sufficient clinical information about the patient must be provided by the referring doctor in order for them to assess the potential benefit. If this cannot be provided then the procedure should not be done. Also, for the protection of the patient, the procedure itself should use the least amount of radiation possible.
The way you prepare for a nuclear medicine procedure depends on the type of exam you are having. To ensure accurate test results, please carefully follow the instructions you receive from the facility where your exam is scheduled or check the list below. When scheduling your exam, be sure to alert your doctor if you have any allergies or special medical problems or needs.
Inform nuclear medicine doctor about your occupation – especially in case of baby sitters, school teachers.
In case of female patients, please inform the doctor in case of suspected pregnancy, whether caring small children, breast feeding. In case of male patients, advice maybe sought on fathering children post radioiodine therapy.
Ask the nuclear medicine doctor for any specific instruction(s) to be followed post procedure.
If the patient works with radioactive materials, or their work is radiation-sensitive, the patient should be advised to inform his or her employer.
In case of discharge after receiving therapy (especially I-131), please get advice from your doctor/RSO regarding using of public transport, resumption of work, visiting crowded public places, having visitors, restrictions to be observed at home.
In case you are planning to travel abroad, ask your nuclear medicine doctor to provide you with written information regarding the nuclear medicine procedure that you have undergone for the purposes of showing to customs/police or other officials.
Radiation safety of patient - Myths debunked

A whole body CT-scan can detect cancer anywhere in the body.
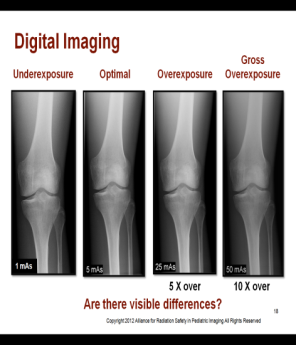
Digital imaging is the best with respect to radiation safety.